Publications
Teratology Primer, 3rd Edition
Can Chemicals in the Environment that Affect Hormone Function Disrupt Development?
Barbara F Hales, McGill University, Montreal, QC, Canada
Robert J. Kavlock, Washington, DC, USA
The endocrine system is made up of glands that produce and secrete hormones; these hormones regulate metabolism, growth and development, tissue function, and sexual function. In the embryo, they play a critical role in regulating the expression of genes that guide the development of a number of organ systems. Changes in either the amount or the timing of hormone exposure can lead to altered human development. For example, humans with a defect in the androgen receptor gene have androgen insensitivity syndrome; although they are genetically male, they have a female appearance, because androgens cannot activate the receptor to masculinize the reproductive tract during critical periods of prenatal development.
Figure 1. The response to an endogenous hormone is depicted on the left. EDCs may enhance (middle) or antagonize (right) the response to this hormone.
https://www.niehs.nih.gov/health/topics/agents/endocrine/index.cfm
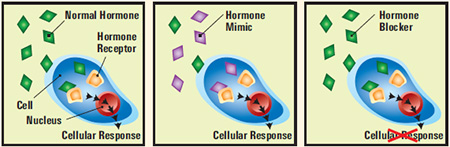
A chemical that disrupts the endocrine system (i.e. an endocrine disrupting chemical or EDC) is defined by the International Programme on Chemical Safety (IPCS), a joint programme of WHO, UNEP and the International Labour Organization as “an exogenous substance or mixture that alters function(s) of the endocrine system and consequently causes adverse health effects in an intact organism, its progeny, or (sub)populations.” A potential EDC is defined as “an exogenous substance or mixture that possesses properties that might be expected to lead to endocrine disruption” (Figure 1). Chemicals that may act as EDCs are found in everyday household products and throughout the environment. Although the mechanisms of action of environmental EDCs may be complex, studies have generally focused on alterations in estrogen, androgen, and thyroid signaling pathways. One of the first hormonally-active chemicals shown to have effects on development in humans was diethylstilbestrol (DES), a synthetic estrogen, given to women during the 1950s in an effort to prevent miscarriage and preterm delivery. In the early 1970s, fetal exposure to DES was linked to vaginal adenocarcinoma, a rare cancer; since then many other effects of maternal DES exposure have been identified. In Taiwan in 1979, many people consumed rice oil contaminated with high levels of polychlorinated biphenyls (PCBs) and dibenzofurans. The offspring of exposed women were smaller at birth and had delays in neurological development. Several more recent studies on PCBs have shown neurological effects in other populations exposed to lower amounts. Although we know that PCBs and related compounds can interact with various components of the endocrine system, the cause for the developmental disorders observed after these exposures is not known.
Our understanding of the potentially harmful effects of EDC exposures during development has advanced tremendously during the past three decades, triggered by the dedication and passion of a number of scientists. In 1992, a publication of the proceedings of a conference organized by Theo Colborn concluded, “We are certain of the following:...A large number of man-made chemicals that have been released into the environment... have the potential to disrupt endocrine systems of animals, including humans.” Since this conference, evidence has accumulated showing that exposure to EDCs may lead to adverse health effects in wildlife living in contaminated environments, in livestock foraging on phytoestrogen-containing plants, in laboratory animal studies, and in humans.
Polybrominated diphenyl ether (PBDE) flame retardants, certain phthalate plasticizers, epoxy resin ingredients, such as bisphenol A (BPA), pesticides, such as methoxychlor and vinclozolin, and even phytoestrogens, such as soy products, may act as EDCs. The PBDEs, added to textiles, plastics, furniture foam and electronic equipment to retard the propagation of flames, leech out into the environment where they are persistent and bioaccumulate. Human exposure to PBDEs is widespread through house dust, air, water and food. In epidemiological studies, the exposure of women during pregnancy to some PBDEs has been associated with effects on measures of intelligence related to learning and memory, such as IQ, in their children. Studies in rodents designed to assess the effects of specific PBDEs on measures that test learning have also demonstrated that these chemicals may act as developmental neurotoxicants. While the mechanism(s) of action of PBDEs as developmental toxicants is not clear, several studies have linked their effects on brain development to thyroid hormone disruption. PBDEs also affect the development of other organs. In humans, there is evidence that PBDE exposure during pregnancy is associated with an increase in the failure of the testes to descend in male infants, a condition known as cryptorchidism. In rodent studies, in utero and lactational PBDE exposure is associated with adverse effects on ovarian folliculogenesis and steroidogenesis in female offspring.
Phthalates, widely used as plasticizers to increase the flexibility of polyvinylchloride (PVC), are found in construction materials, toys, packaging films and medical devices. They leech out of these products and are ubiquitous environmental contaminants. In animal studies, exposure to certain phthalates (e.g. to di(2-ethylhexyl) phthalate, DEHP; dibutyl phthalate, DBP; benzylbutyl phthalate, BzBP) during a specific window of development may have adverse effects on the reproductive system of offspring. In male animals, these effects include decreases in testosterone production and in anogenital distance, an increase in the incidence of hypospadias and the presence of multi-nucleated early male germ cells (gonocytes) in the testis. As with the earlier examples, the precise mode of action of members of this chemical class is not clear, but the observed phenotypes are consistent with alterations in hormonal signaling in the developing organism. In parallel, some human studies suggest that increases in maternal urinary concentrations of metabolites of di(2-ethylhexyl) phthalate (DEHP) are associated with a shorter anogenital distance in male infants.
The epoxy resin ingredient bisphenol A (BPA) is found in the protective linings of metal-based food and beverage cans and in some reusable polycarbonate water bottles, tableware, and food storage containers. Exposure to BPA is widespread – data from the Canadian Health Measures Survey (2007-2013) and NHANES reveal that BPA is detected in the urine of more than 90% of those tested. Perhaps this finding is not surprising since it has been estimated that approximately 16,000 processed food and drink items are packaged in materials that may contain BPA. BPA has been reported to have estrogen-like activity. In animal studies, BPA exposure has been reported to lead to a disruption of estrous cyclicity, the early onset of puberty, a reduction in the sexual dimorphism of brain structures, effects on mammary glands, changes in the prostate, a reduction in sperm counts and infertility, in addition to obesity. Furthermore, there is evidence that some of the effects of BPA may not be limited to exposed individuals, but may be carried into the next generation. Epidemiological studies link environmentally relevant BPA exposures with adverse effects in humans. For example, prenatal BPA exposure has been associated with effects on fertility, neurobehaviour, and obesity. During pregnancy, elevations in urinary BPA concentrations have been associated with a reduction in TSH levels and an increase in biomarkers of inflammation and oxidative stress.
We may not fully appreciate the impact of endocrine disruptors in the environment on human health since many of the effects of hormone disruption are not obvious at birth, only becoming apparent on the functional level as the individual matures. This realization has led to an urgency to increase our understanding of the effects of endocrine active chemicals. For example, the US Environmental Protection Agency initiated an Endocrine Disruptor Screening Program (EDSP) (https://www.epa.gov/endocrine-disruption/what-endocrine-disruption) to screen pesticides, chemicals, and environmental contaminants for their potential effect on estrogen, androgen, and thyroid hormone systems. However, in its more than 15 years of existence to date, relatively few of the thousands of chemicals covered by this program have been screened for endocrine activity, due in part to the difficulties in establishing validated assays and the cost of screening. This program recently adopted a high throughput screening system for estrogenic activity that has the potential to examine large numbers of chemicals of interest (See: https://www.epa.gov/endocrine-disruption/use-high-throughput-assays-and-computational-tools-endocrine-disruptor).
Today, human, animal, and cell-based research data that provide evidence that EDCs chemicals affect human health and the ecosystem are available; these data have led numerous organizations, including the Endocrine Society, the World Health Organization (WHO), the United Nations Environment Programme (UNEP), and the American Medical Association to call for prevention policies and regulatory actions by governments, or voluntary withdrawal by industry due to public pressure. For instance, Parties of the Stockholm Convention on Persistent Organic Pollutants (POPs) banned the tetra-, penta-, hexa-, and hepta-BDE flame retardants in 2009. Numerous jurisdictions, including Canada, the USA, and the European Union, have introduced standards and/or regulated the use of specific phthalates and BPA in certain infant products. In some instances, these regulations have been passed in the absence of a complete understanding of the modes of action of these chemicals. To fill the void created by the withdrawal of these products, new chemicals are introduced to meet industry needs. The nature of these alternative materials is often not disclosed; indeed, there is usually very little information about alternatives, including what they are or whether they are any safer than the compounds they are replacing. While it is evident that replacement chemicals are often chosen on the basis of their physico-chemical properties and their functional suitability, e.g. as a flame retardant, plasticizer, or can liner, it is also crucial that the impact of these alternatives on human and environmental health be considered with great care. The Organisation for Economic Co-operation and Development (OECD) has identified a number of gaps in the current landscape of alternatives assessment practices and opportunities to enhance alternatives assessment practices (http://www.oecd.org/env/ehs/testing/oecdworkrelatedtoendocrinedisrupters.htm).
Information on EDCs and their possible adverse health effects is now widely available online (See: https://youtu.be/J9SWBAUIAvw; https://www.niehs.nih.gov/health/topics/agents/endocrine/index.cfm) along with general advice from an advocacy group to pediatricians and the public on how to avoid or minimize exposure to EDCs (See: https://www.nrdc.org/stories/9-ways-avoid-hormone-disrupting-chemicals).
Suggested Reading
Barlow S, Kavlock RJ, Moore JA, Schantz SL, Sheehan DM, Shuey DL, Lary JM. Society for Birth Defects Research and Prevention Public Affairs Committee position paper: developmental toxicity of endocrine disruptors to humans. Teratology. 1999 60(6):365-75.
Colborn, T and Clement, C, (eds.) Chemically-Induced Alterations in Sexual and Functional Development: The Wildlife/Human Connection. Volume XX1 of Advances in Modern Environmental Toxicology, Princeton, NJ: Princeton Scientific Publishing Co., 403 pp,. 1992.
Committee on Endocrine-Related Low-Dose Toxicity. National Academies of Sciences, Engineering, and Medicine. 2017. Application of Systematic Review Methods in an Overall Strategy for Evaluating Low-Dose Toxicity from Endocrine Active Chemicals. Washington, DC: The National Academies Press. ISBN: 978-0-309-45862-7. https://doi.org/10.17226/24758.
Diamanti-Kandarakis, E., Bourguignon J-P, Giudice L.C., Hauser R., Prins G.S., Soto A.M., Zoeller R.T. and Gore A.C. Endocrine- Disrupting Chemicals: An Endocrine Society Scientific Statement Endocrine Reviews 2009: 30 (4):293–342
Gray LE. Twenty-five years after “Wingspread” – Environmental endocrine disruptors (EDCs) and human health. Current Opinion in Toxicology 2017 3:40-47
International Programme on Chemical Safety 2002. Global Assessment of the State-of-the-Science of Endocrine Disruptors. Geneva:World Health Organization. http://www.who.int/ipcs/publications/new_issues/endocrine_disruptors/en/
Kavlock, R.J., Daston, G. P., DeRosa, C., Fenner-Crisp, P., Gray, L. E., Kaattari, S., Lucier, G., et al. (1996). Research needs for the risk assessment of health and environmental effects of endocrine disruptors: a report of the U.S. EPA-sponsored workshop. Environmental Health Perspectives, 104 Suppl 4(Suppl 4), 715–740.
Lam J, Lanphear BP, Bellinger D, Axelrad DA, McPartland J, Sutton P, Davidson L, Daniels N, Sen S, Woodruff TJ. Developmental PBDE Exposure and IQ/ADHD in Childhood: A Systematic Review and Meta-analysis. Environ Health Perspect. 2017 Aug 3;125(8):086001
OECD Alternatives Assessment Guidance. http://www.oecdsaatoolbox.org/Home/AAGuides
Rotroff DM, Dix DJ, Houck KA, Knudsen TB, Martin MT, McLaurin KW, Reif DM, Crofton KM, Singh AV, Xia M, Huang R, Judson RS. Using in vitro high throughput screening assays to identify potential endocrine-disrupting chemicals. Environ Health Perspect. 2013: 121(1):7-14.
Science for Policy report by the Joint Research Centre (JRC), the European Commission’s science and knowledge service. Screening methodology to identify potential endocrine disruptors according to different options in the context of an impact assessment. http://publications.jrc.ec.europa.eu/repository/bitstream/JRC101950/jrc%20screening%20methodology%20for%20ed%20impact%20assessment%20%28online%29.pdf
US EPA Endocrine Disruptor Screening Program Test Guidelines. https://www.epa.gov/test-guidelines-pesticides-and-toxic-substances/series-890-endocrine-disruptor-screening-program
Wong, KH, Durrani TS. Exposure to Endocrine Disrupting Chemicals in Consumer Products – A guide for Pediatricians. Curr Probl Pediatr Adolesc Health Care 2017 47:107-118.